The past year has put the spotlight on clinical trials as we all eagerly awaited updates on the development of COVID-19 vaccines. However, as high profile as these trials were, and as quick as pharmaceutical companies managed to make the process, it is important to remember that there are hundreds of other trials taking place all the time for life saving medicines. And this complex, normally drawn-out process, is at an inflection point where speed versus practicality needs to be reviewed.
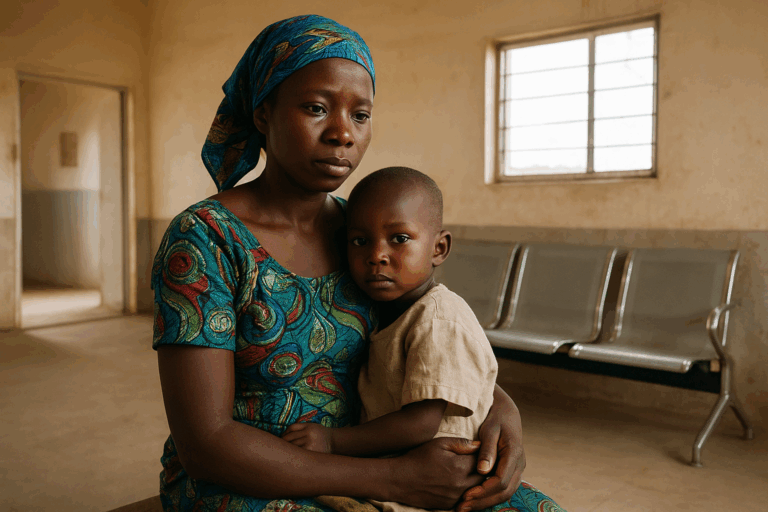
One of the biggest challenges with traditional clinical trials is that they depend on recruiting and retaining volunteers and patients, something that can be costly and logistically demanding. However, as we have seen this year, when we come together as a global community, evolving the traditional trial model can lead to amazing results. From this, the pharmaceutical industry needs to seek inspiration. They need to embrace new, innovative approaches to clinical trials.
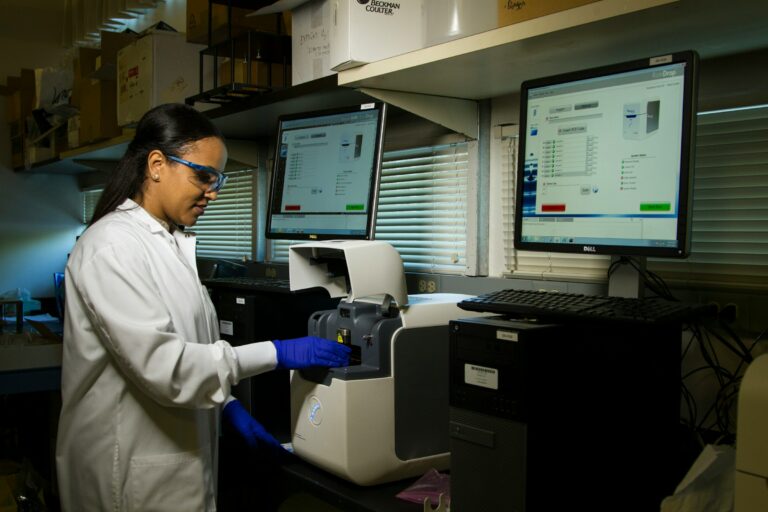
A big shift that is currently gaining ground is the idea of decentralised trials, where the process is moved away from centering around a physical medical facility and instead goes to where the patients are. Flipping this focus is being made increasingly easier thanks to technology. AI, machine learning and cloud computing are behind this drive to put patients at the centre of trials across the healthcare system.
Less complexity, more impact
Huge paperwork and lots of travel have traditionally acted as roadblocks to large uptake in clinical trials. In recent times, fears of attending appointments in a healthcare setting where there is a perceived risk of being infected by coronavirus have also proved a challenge. These issues don’t stop after the recruitment drive either. Managing patients to stay on-board and avoiding poor protocol adherence is another major problem affecting the conclusiveness of many clinical trials.

Tech is leading the way
Moving to decentralised clinical trials won’t happen overnight. A hybrid approach is more likely, which balances onsite patient and remote visits. But the pandemic has certainly accelerated acceptance by medical professionals that new technologies and devices can, and should, be used to safely conduct decentralised trials.
Wearable devices is one area in particular which demonstrates great potential. Whether these are worn on the wrist, or as a patch on the body, AI-embedded capabilities allow a device to measure a patient’s heart rate or metabolism remotely. These can be linked through secure networks which allow clinicians to pick up the data and analyse it in real time.
There’s no ‘one-size-fits-all approach’ to this. Different trials require the adoption of different technologies – all of which can be mapped out by digital strategies. That being said, an ecosystem of technologies to support decentralised trials, such as video calling and electronic reminders, can certainly improve patient compliance in trials. From making sure participants take medication at the right time, to prompting them to log down developments in their diary and remember when to attend remote check-ins, the move to digital can help to improve patient morale and adherence during the process. This can lead to more accurate results.
Better data equals better results
To be successful, clinical trials depend on capturing interoperable data and combining it with medical research. Doing this allows researchers to show evidence of benefit to patients, along with any potential side effects – which can later be submitted to regulatory agencies.
Crucial to this is that the data is accurate. That means all of the data – whether it’s numbers of patient dropouts, adverse reactions, frequency and nature of data collection, must be tracked, logged and analysed. This, however, requires Herculean coordination of the pharmaceutical industry, physicians and patients to generate valid evidence. But the issue is made more complex given there’s no universal standards for medical devices. Any device measuring heart rate or respiration rate, for example, requires calibration and a sophisticated degree of understanding. This adds to the challenge of effectively managing the plethora of different platforms and data sources, as well as ensuring the patient data is high quality, safe and secure.
A significant incentive for decentralised trials is the collection of real-world data, and real-world evidence, which provide an assessment over the lifetime of a trial. With the use of various different technologies, decentralised trials can collect more data from patients than at traditional site-based clinical studies. Because these technologies can deliver data straight from the source, such as a wearable device, they also reduce the need for additional data verification, speeding up and reducing the cost of clinical trials.
Planning for the future
The pharmaceutical industry is no stranger to embracing new technology, but rarely has it been focused around the patients. But now is an inflection point. The pandemic has forced greater innovation and greater understanding of patient needs upon pharma companies.
Moving forward, and preparing for the possible increased frequency of black swan events, trials must put convenience and flexibility at the centre of the work. From recruitment and engagement, to monitoring and data capture, everything has to come with ease to the patients. Decentralised trials offer a shield against disruption and offer continuity of operations that so many rely on for critical medical advancement.

Carolina Wosiack
Managing Director, EMEA at CI&T